Introduction
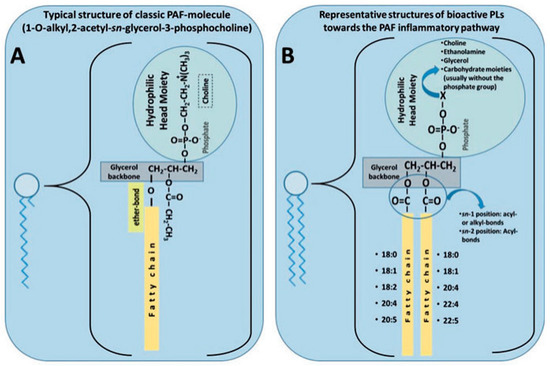
Non-communicable diseases (NCD) are a significant burden on health care systems and society. Atherosclerotic cardiovascular diseases (ASCVD or CVD) are one of the main NCDs and are the leading cause of death worldwide. Previously considered a lipid storage disease, CVD is now thought to be far more complex, encompassing a significant pro-inflammatory state, dysregulated lipid metabolism, and oxidative stress [1]. Over half of the deaths related to cardiometabolic diseases are attributed to maladaptive diet [2,3]. Many diets and various dietary constituents have been strongly linked with beneficial effects against CVD [3]. One family of molecules of significant interest for their pro-inflammatory role in CVD and NCD is platelet-activating factor (PAF) and PAF-like lipids. Notably, these lipids have garnered significant attention for their potential modulation by pharmacological and dietary intervention [4,5]. The purpose of this paper is to highlight the role of inflammation in CVD, and considering that diet and lifestyle are modifiable risk factors for CVD prevention, we aim to explore the role that dietary polar lipids (PL) play against inflammation and the onset of CVD via the role of PAF.
Inflammation, Atherosclerosis, and Cardiovascular Diseases
And the continuation of the story on omega-3 fatty acids and inflammation (our latest publication; in review : Marine Drugs)
Cardiovascular diseases (CVD) remain the leading cause of death across the globe, hence, establishing strategies to counteract CVD are imperative to reduce mortality and the burden on health systems. Dietary modification is an effective primary prevention strategy against CVD. Research regarding dietary supplementation has become increasingly popular.
This review focuses on the current in vivo, in vitro, and epidemiological studies associated with that of omega-3 polyunsaturated fatty acids (n-3 PUFA) and polar lipids (PLs) and how they play a role against CVD.
Furthermore, this review focuses on the results of several major clinical trials examining n-3 PUFA regarding both primary and secondary prevention of CVD. Notably, we place a lens on the REDUCE-IT and STRENGTH trials. Finally, supplementation of PLs has recently been suggested as a potential alternative avenue for the reduction of CVD incidence versus neutral forms of n-3 PUFA. However, the clinical evidence for this argument is currently rather limited.
Therefore, we draw on the current literature to suggest future clinical trials for PL supplementation. We conclude that despite conflicting evidence, future human trials must be completed to confirm whether PL supplementation may be more effective than n-3 PUFA supplementation to reduce cardiovascular risk.