Omega-3 fatty acids and the question of polarity
Since the conception that fish has strong anti-thrombotic activities, omega-3 fatty acids were thought to have strong bioactivities in lowering the so-called Cardiovascular Risk (CR).
The whole story started on the potential value of these acids in relation to CR and the development of Cardiovascular Diseases (CVD). Back in 1976, where the diet of Inuit Eskimos came under the microscope of scientists and an examination of the composition of Eskimo food was carried out in north western Greenland. The scientists collected duplicate specimens of diets from 50 adults (25 males and 25 females) and these samples were analysed for water, ash, protein, fat, individual fatty acids, cholesterol, and carbohydrate. These results were compared with those of typical Danish diets. We would need to highlight here, that Eskimo diet is mainly seal and fish, therefore, the Eskimo’s fish intake is very high. Clear differences between Eskimo and Danish food were found. The Eskimo diets were richer in polyunsaturated fatty acids, the ratio to saturated fatty acids was 0.84 as compared with 0.24 in Danes. The polyunsaturated fatty acids were predominantly of the linolenic class (OM3FA) in Eskimos and the linoleic class (OM6FA) in Danes. Fatty acids with one double bond than palmitoleic and oleic acids were high in Eskimo diets, but negligible in Danish. The results were correlated to previous examinations of the plasma lipids in Eskimos. The rarity of ischemic heart disease in Greenland Eskimos may partly be explained by the antithrombotic effect of the long-chained polyunsaturated fatty acids, especially eicosapentaenoic acid (EPA) prevalent in diets rich in marine oils. And this was the first study that linked EPA to reduced rates of CVD, published in 1980.
Is this though the whole picture? Did we make any mistakes in making these assumptions? To answer these questions, we need to think about the structures of fatty acids in fish. The fatty acids are not present in marine food and fish as free fatty acids but as derivatives (see our relevant paper here).
Polarity of fatty acids : why is polarity very important?
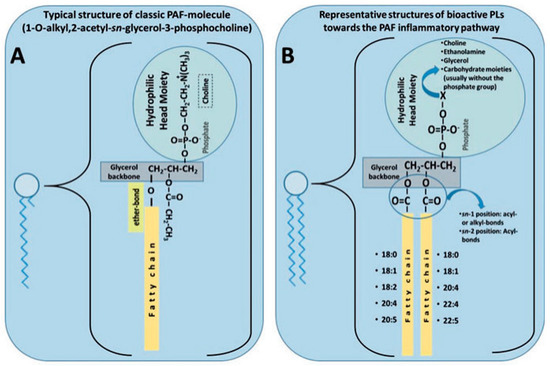
From a chemical perspective, marine phospholipids are derivatives of glycerol where at carbons 1 and 2 of glycerol, we have esterified a range of different fatty acids and at carbon 3, there is a phosphate group with a hydrophilic head-group (Q). The acids that can be present at carbons 1 and 2 are given in figure 3.6. We would need to note here that for each acid there are two numbers: the first number is the number of carbons, and the second number is the number of double bonds, e.g. 18:0 is a fatty acid with 18 carbons and zero double bonds while 22:5 is a fatty acid with 22 carbons and 5 double bonds.
The most common structures of phospholipids are depicted here: phospholipids with a glycerol backbone (GPLs); sphingomyelin as a representative of a sphingosine-backbone phospholipid (SPLs); and alkyl-phospholipids (Alkyl-GPLs) that have a fatty chain linked with an ether-bond at the sn-1 position of the glycerol backbone.
From a biochemical perspective, the presence of the phosphate group and the hydrophilic head group (Q) in the marine phospholipids renders them more polar than the esters of OM3FA or free acids (figure 3.5) and this higher polarity makes them more labile and capable to reach the blood flow much more efficiently than the esters or the acids of figure 3.5. This difference in polarity is of fundamental importance in terms of bioefficacy in relation to thrombosis and reducing CR.
Where do we stand today?
In our latest publication (here), we present all the latest evidence on the cardioprotective properties of neutral and polar fatty acids.
In our review paper, we review focus on the current in vivo, in vitro, and epidemiological studies associated with that of omega-3 polyunsaturated fatty acids (n-3 PUFAs) and polar lipids (PLs) and how they play a role against CVD. Furthermore, this review focuses on the results of several major clinical trials examining n-3 PUFAs regarding both primary and secondary prevention of CVD. Notably, we place a lens on the REDUCE-IT and STRENGTH trials. Finally, supplementation of PLs has recently been suggested as a potential alternative avenue for the reduction of CVD incidence versus neutral forms of n-3 PUFAs. However, the clinical evidence for this argument is currently rather limited. Therefore, we draw on the current literature to suggest future clinical trials for PL supplementation. We conclude that despite conflicting evidence, future human trials must be completed to confirm whether PL supplementation may be more effective than n-3 PUFA supplementation to reduce cardiovascular risk.
Moving forward to produce a supplement strong in reducing cardiovascular risk
In the n-3 PUFA research space, many large clinical trials have been conducted with variable results because of differing trial design, placebos used, doses, and the form of n-3 PUFA consumed. An in-depth review of the REDUCE-IT and STRENGTH trials was conducted. Generally, while n-3 PUFAs may provide some cardiovascular benefits, large-scale trials have failed to conclusively support their use for cardiovascular risk reduction. This is largely due to differences in trial design, placebo use, and the different forms of n-3 PUFAs that have been assessed. The consumption of n-3 PUFA supplements is high worldwide but likely poses limited risk for adverse events.
Trials largely expressed concerns about the increased incidence of atrial fibrillation, which should be monitored closely at a population level.
In our review, we evaluated the role and potential of n-3 PUFAs withing dietary PLs and their potential cardiovascular benefits for risk reduction, through the examination of both in vitro and in vivo studies. Evidence regarding PL supplementation, although promising, is limited and further research is required. Given the large gaps within the literature remaining for both n-3 PUFAs and PLs, it is difficult to draw concrete conclusions. In designing future studies, we suggest that the form of n-3 PUFA used needs to be taken into account along with the choice of placebo. Studies investigating PL forms of n-3 PUFAs are also warranted in humans to determine whether the polar head group conveys greater bioavailability of n-3 PUFAs, thus increasing their efficacy and potency.